- Describe schizophrenia and categorize its symptoms
- Describe genetic, biological, and environmental factors that are associated with the development of schizophrenia
- Identify and differentiate the symptoms and potential causes of various dissociative disorders
schizophrenia
Schizophrenia is a devastating psychological disorder that is characterized by major disturbances in thought, perception, emotion, and behavior. Its most common symptoms include hallucinations and delusions. Schizophrenia is considered a psychotic disorder, or one in which a person becomes detached from reality—a person’s thoughts, perceptions, and behaviors are impaired to the point where they disrupt typical life functioning.
Schizophrenia is not a condition involving a split personality; that is, schizophrenia is not the same thing as dissociative identity disorder (better known as multiple personality disorder). These disorders are sometimes confused because the word schizophrenia first coined by the Swiss psychiatrist Eugen Bleuler in 1911, derives from Greek words that refer to a “splitting” (schizo) of psychic functions (phrene) (Green, 2001).
About 1% of the population experiences schizophrenia in their lifetime, though global estimates are even lower, with lifetime prevalence between 0.3% and 0.7% (WHO, 2025). The disorder is typically first diagnosed during early adulthood (late teens and early to mid-20s).
The disorder significantly impacts daily functioning, including maintaining employment, managing finances, self-care, and relationships. Even with the best available treatments, many individuals continue to experience substantial social and occupational challenges throughout their lives.
Recent research conceptualizes schizophrenia as a heterogeneous syndrome rather than a single disease entity—a complex, multi-dimensional condition with varying degrees of psychotic, negative, cognitive, mood, and motor manifestations (Tandon et al., 2024).
Symptoms of Schizophrenia
The main symptoms of schizophrenia include hallucinations, delusions, disorganized thinking, disorganized or abnormal motor behavior, and negative symptoms.
hallucination
A hallucination is a perceptual experience occurring without external stimulation. Auditory hallucinations—hearing voices—occur in roughly two-thirds of patients and are the most common form (Andreasen, 1987). These voices may be familiar or unfamiliar, may converse or argue, or may provide running commentary on the person’s behavior (Tsuang, Farone, & Green, 1999).
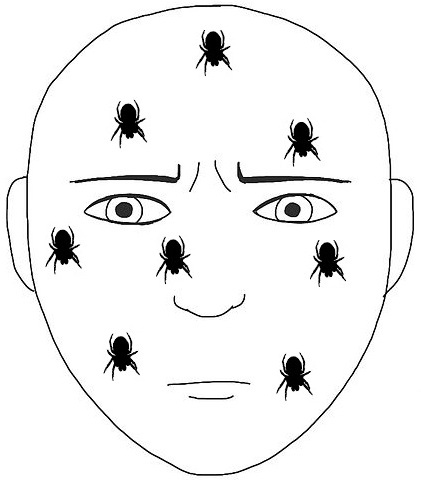
Less common forms include visual hallucinations (seeing things that aren’t there), olfactory hallucinations (smelling nonexistent odors), and tactile hallucinations (such as feeling imaginary insects crawling on the skin).
delusions
Delusions are firmly held beliefs contrary to reality that persist despite contradictory evidence. While many people hold beliefs others might consider unusual, delusions are clearly implausible or absurd. Types of delusions include:
- Paranoid delusions: False beliefs that others are plotting harm—such as believing a family member is collaborating with government agencies to poison them
- Grandiose delusions: Beliefs of having special powers, unique knowledge, or extraordinary importance—such as claiming to be a historical figure or possessing ancient wisdom
- Thought withdrawal/insertion: Beliefs that thoughts are being removed from or placed into one’s mind
- Somatic delusions: Beliefs about abnormal bodily experiences—such as believing internal organs are being consumed by insects
disorganized thinking
Disorganized thinking refers to disjointed, incoherent thought processes—typically evident through speech. A person might ramble, exhibit loose associations (jumping randomly between topics), or produce speech so disorganized it seems like random word combinations.
This symptom also includes blatantly illogical statements (e.g., “The stadium is in the city. I live in the city. Therefore, I live at the stadium.”) and tangentiality—responding with statements barely related to what was said. For example, when asked about job training, a person might respond about riding a train, linking the two through superficial word association.
disorganized motor behavior
Disorganized or abnormal motor behavior includes unusual movements and actions: becoming unusually active, displaying child-like behaviors (giggling, self-absorbed smiling), engaging in repetitive purposeless movements, or showing odd facial expressions.
In severe cases, catatonic behaviors may occur—decreased reactivity to the environment, including posturing (maintaining rigid, bizarre positions for extended periods) or catatonic stupor (complete lack of movement and verbal response).
Positive and Negative Symptoms
Schizophrenia symptoms are categorized as positive or negative.
Positive Symptoms
Positive symptoms are symptoms of commission—behaviors or experiences added to normal functioning. These include hallucinations, delusions, disorganized speech, and bizarre behaviors described above.
Negative Symptoms
Negative symptoms reflect decreases and absences in typical behaviors, emotions, or drives (Green, 2001):
- Diminished emotional expression (flat affect): Showing no emotion in facial expressions, speech, or movements when such expression would normally occur
- Avolition: Lack of motivation for self-initiated, meaningful activity—including basic tasks like personal hygiene
- Alogia: Reduced speech output; patients simply don’t say much
- Asociality: Social withdrawal and disinterest in social interactions
- Anhedonia: Inability to experience pleasure from activities most people find enjoyable—hobbies, recreation, or social activities
Forensic Psychology
In August 2013, 17-year-old Cody Metzker-Madsen attacked foster sibling 5-year-old Dominic Elkins on his foster parents’ property. Believing that he was fighting goblins and that Dominic was the goblin commander, Metzker-Madsen beat Dominic with a brick and then held him face down in a creek. Dr. Alan Goldstein, a clinical and forensic psychologist, testified that Metzker-Madsen believed that the goblins he saw were real and was not aware that it was Dominic at the time. He was found not guilty by reason of insanity and was not held legally responsible for Dominic’s death (Nelson, 2014).
Cody was found to be a danger to himself or others. He remains in a psychiatric facility and will continue to do so until he is judged to be no longer dangerous. Metzker-Madsen was again charged with attacking his roommate in the mental hospital in 2024.
According to the American Psychiatric Association, individuals who are found not guilty by reason of insanity are often confined to psychiatric hospitals for as long or longer than they would have spent in prison for a conviction.
Most people with mental illness are not violent. Only 3–5% of violent acts are committed by individuals diagnosed with severe mental illness, whereas individuals with severe mental illnesses are more than ten times as likely to be victims of crime (MentalHealth.gov, 2017). The psychologists who work with individuals such as Metzker-Madsen are part of the subdiscipline of forensic psychology.
Forensic psychologists are involved in psychological assessment and treatment of individuals involved with the legal system. They use their knowledge of human behavior and mental illness to assist the judicial and legal system in making decisions in cases involving such issues as personal injury suits, workers’ compensation, competency to stand trial, and pleas of not guilty by reason of insanity.